In the not-too-distant future, envision a world where checking in on the well-being of our loved...
Comparison of Camera-Acquired Vital Signs to Conventional Vital Signs in a Space-Analog Environment
Abstract
Introduction
Vital sign acquisition is a key component of modern medical care. In wilderness and space medical settings, vital sign acquisition can be a difficult process because of limitations on available personnel or lack of access to the patient. Camera-acquired vital signs could address each of these difficulties.
Methods
Healthy volunteers used software designed by Presage Technologies to acquire heart rate and respiratory rate at the HI-SEAS space-analog site in Mauna Loa, Hawai’i. Camera-acquired vital signs were compared to more conventionally acquired vital signs.
Results
Camera-acquired heart rate showed high correlation to conventionally acquired heart rate (R ∼ 0.95). Camera-acquired respiratory rate showed moderate correlation (R ∼ 0.65).
Conclusions
These results show that camera acquisition of vital signs is theoretically feasible in wilderness and space-analog environments. HR may be highly accurate even using current technology. Additional studies will be needed to further validate other types of camera sensors and other potential environments such as partial gravity and microgravity.
Introduction
Vital signs constitute a key component of medical care in most modern medical settings. These five metrics (heart rate, respiratory rate, blood pressure, temperature, and pulse oximetry) can be key indicators of a patient's degree of illness and response to various therapies. As such, vital signs play key roles in patient triage, treatment, and disposition. Vital signs have been shown to predict patient outcomes as wide-ranging as morbidity, mortality,1 transfer to a higher level of care,2 and need for readmission when discharged.3
Despite their importance, the acquisition of vital signs can be delayed in emergency departments and other conventional medical settings. Studies have shown that factors such as nurse staffing ratios4 and crowding5can lead to decreased frequency of vital sign measurements. Some studies have shown vital sign updates occur as infrequently as only once every 2 hours.6 Many emergency departments are seeking to address this deficiency through a variety of quality-improvement initiatives. Of note, in modern telemedical care, patients may have no physical contact with a medical provider. Some studies have sought to assess the feasibility of patients self-reporting vital signs in those environments.7
Vital signs are even more important in wilderness, military, and other austere settings. There, a lack of access to laboratory testing, imaging, and other medical diagnostics often leaves vital signs as the sole objective marker of a patient's degree of illness. Spaceflight may be the most austere of these environments. All medical resources sent in spaceflight must be considered carefully for cost, mass, volume, and ease of use. Astronauts, often not medical experts, must also receive training in the use of medical resources. With this in mind, simpler, more reusable medical resources would be preferred. In addition, monitoring vital signs during astronaut exercise is often used for research purposes and to ensure each astronaut gets an adequate exercise prescription. However, wearable sensors are often described as uncomfortable, and movement can make them unreliable.8
In the past few years, multiple research groups have begun to validate non-contact vital sign acquisition in terrestrial environments.9 These studies, usually of camera-acquired vital signs, could potentially improve both single-patient care and clinical system function. Other groups have attempted to test wearable vital sign sensors for potential use in spaceflight.10 Here, we present our experience using a simple iPhone (™) application to acquire heart rate (HR) and respiratory rate (RR) using phone cameras at a space analog site.
Methods
Six healthy astronaut analog volunteers were recruited on a convenience basis at the high-altitude Hawai’i Space Exploration Analog and Simulation (HI-SEAS) habitat in Mauna Loa, Big Island, Hawaii. Three participants were male, three were female, and their ages ranged from 18–52 years old. Measurements were taken multiple times over the course of a six-day simulated spaceflight. Measurements were taken at rest, after exercise, and after simulated extra-vehicular activity. Measurements were also taken in either a designated “medical room” or in other locations throughout the habitat.
Camera-acquired HR and RR were obtained using Presage Technologies11 software installed on an iPhone device. This process involved activating the software and placing the patient's face within the camera's field of view. HR and RR were calculated based on pulse plethysmography measurement and chest wall movement, respectively. No physical contact with the subject was required during this time. Data processing occurred on the phone itself, and readouts were provided within about 30 seconds. These values are subsequently referred to as App HR and App RR.
Conventionally acquired HR was acquired with a portable digital pulse oximeter. Conventionally acquired RR was acquired through visual measurement by an observer over 30 seconds, then doubled to calculate the minute rate. These values are subsequently referred to as Measured HR and Measured RR.
These values were then compared using a Student's t-test and standard linear regression.
Results
Sixty measurements were made over the course of six days (averaging about ten measurements perparticipant.) Of note, 59 of these were in the seated position, and one was in the supine position.
Figure 1 and Table 1 compare App HR and Measured HR. Overall, App HR was highly correlated to Measured HR. The mean difference was about 1 beat/minute. The Pearson correlation coefficient was extremely high, at 0.946.
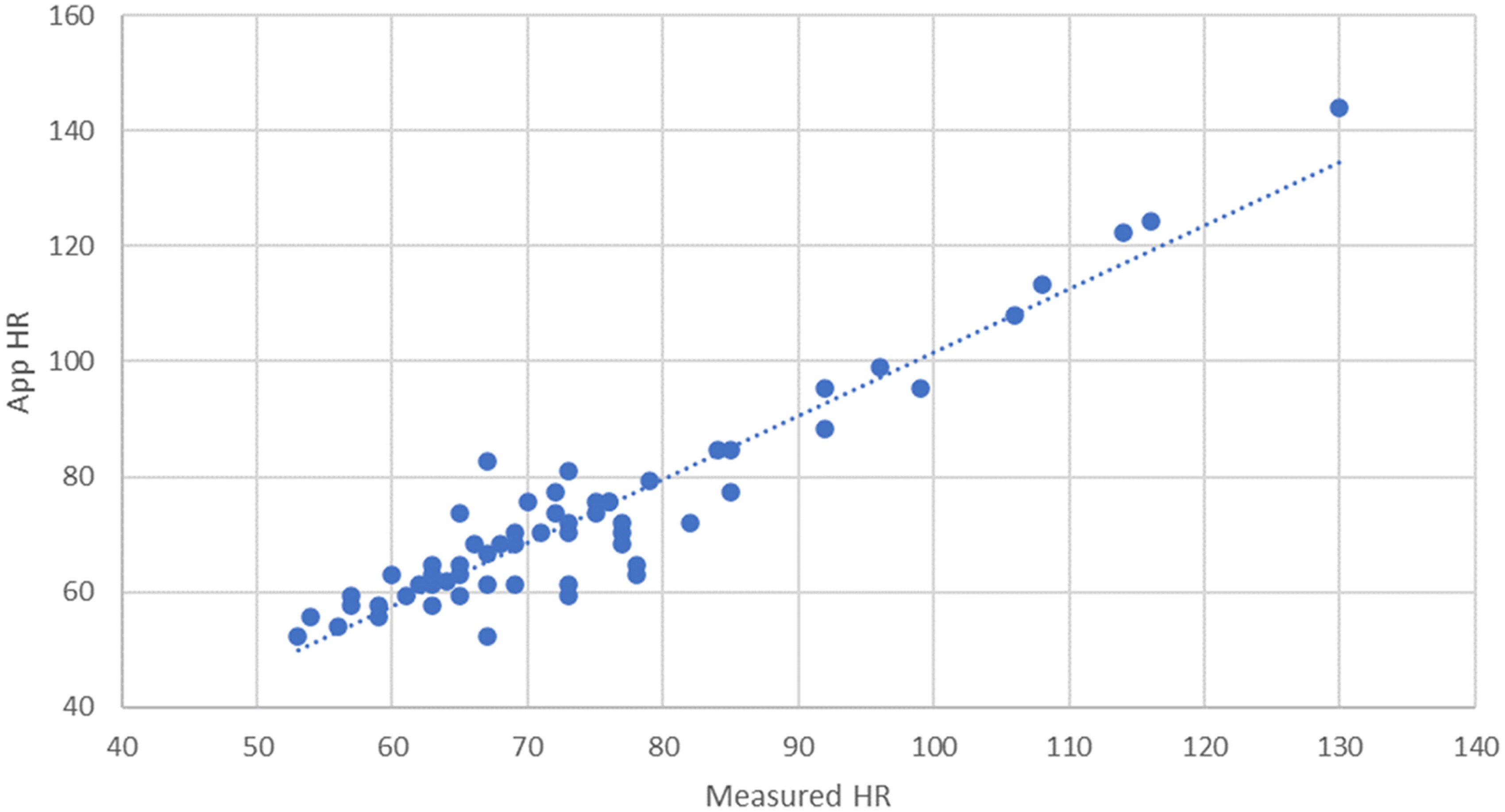
| Mean difference (App HR – Measured HR) | −0.96 |
| Standard error | 0.80 |
| Interquartile range | (−3.65, 1.85) |
| Correlation coefficient | 0.946 |
Figure 2 and Table 2 compare App RR and Measured RR. Here, moderate correlation was present. The mean difference was about 0.5 breaths/minute, with a Pearson correlation coefficient of 0.652.
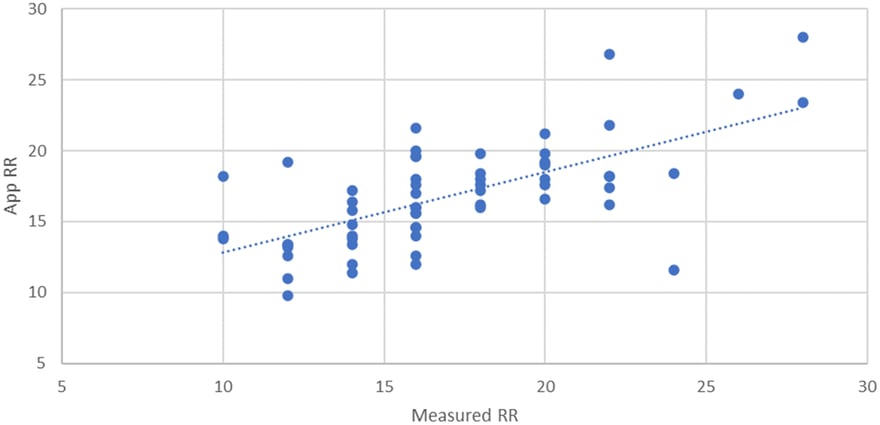
| Mean difference (App RR – Measured RR) | −0.227 |
| Standard error | 0.43 |
| Interquartile range | (−2.0, 1.45) |
| Correlation coefficient | 0.652 |
Each study participant interacted with the application, and all participants anecdotally found it intuitive and easy to use. There were occasional issues with ambient lighting, subject movement, or facial positioning. These could be addressed through increasing the ambient lighting and repositioning of the subject. For one measurement, the app appeared to freeze on data collection and also required a reset.
Discussion
Overall, these data suggest that HR can be reliably acquired using a non-contact smartphone application at a high-altitude space analog simulation site. RR can also be acquired in this manner, though it may have more errors.
Of note, study participants did note visual observation of the respiratory rate was itself difficult and may have led to error. Studies have shown that different manual measurements of RR have an intraclass correlation coefficient of 0.64, similar to the correlation between manual measurements and cameras seen in this study.12 The US Food and Drug Administration (FDA) itself has recommended the use of an absolute difference in RR (+/–2 BPM) rather than correlation to assess the accuracy of medical devices measuring RR.13 Using that standard, 36/60 measurements, or 60%, would meet the FDA standard for accuracy. Other studies have used an absolute difference of 4 BPM to assess accuracy.12 At that standard, 51/60, or 85%, would be considered accurate.
We acknowledge that this is a small pilot study only showing the feasibility of using this type of technology in austere and space-analog environments. No formal power calculations were performed, as the goal of the work was to demonstrate the engineering endpoint of adequate data capture processes. As this was not a systematic health study, no statistics were required to meet the engineering goal. Future studies are planned that will address systematic health parameter evaluations.
Further, our study calculates HR via pulse, a measurement of force transmission through the blood vessels. While HR and pulse are essentially interchangeable throughout normal heart rate and blood pressure ranges, this may not be the case at more extreme values. The current gold standard measurement for HR is electrocardiography (EKG). Future studies could compare camera-acquired HR to EKG-measured HR instead of pulse.
Future studies could potentially be expanded in multiple other new directions, including measurement of time required for vital sign measurement or measurement of vital signs during movement or active exercise. The camera used to acquire vital signs could also be varied to include fixed sensors more representative of spaceflight environments or integration into helmets as might be seen in military medicine. Additionally, while this study was performed at ∼8200 ft of altitude at the HI-SEAS habitat, this still occurred at normal terrestrial gravity of roughly 1G. Further studies will need to validate this technology in partial-gravity and zero-gravity environments.
Conclusion
Our study shows the feasibility of using a smartphone application to acquire HR and RR in wilderness and space-analog environments. Use of this type of non-contact measure could potentially improve the frequency of vital sign measurements in both conventional and austere medical settings. Specific to spaceflight, this technology could both expand and simplify medical resources available to future astronauts.
Declaration of Conflicting Interests
IRB: This study follows policies issued by the Baylor College of Medicine and was reviewed with experienced research staff. As a small engineering study that used volunteers to test data capture processes only, this study did not require IRB review.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Carlo A. Canepa https://orcid.org/0009-0001-5723-0128
Amit S. Padaki https://orcid.org/0000-0002-2689-2233
References
1. Candel BG, Duijzer R, Gaakeer MI, et al. The association between vital signs and clinical outcomes in emergency department patients of different age categories. Emerg Med J. 2019; 39(12): 903–11.
2. Hodgson NR, Poterack KA, Mi L, et al. Association of vital signs and process outcomes in emergency department patients. West J Emerg Med. 2019; 20(3): 433.
3. Gabayan GZ, Gould MK, Weiss RE, et al. Emergency department vital signs and outcomes after discharge. Acad Emerg Med. 2017; 24(7): 846–54.
4. Redfern OC, Griffiths P, Maruotti A, et al. The association between nurse staffing levels and the timeliness of vital signs monitoring: a retrospective observational study in the UK. BMJ Open. 2019;9(9):e032157.
5. Depinet HE, Iyer SB, Hornung R, et al. The effect of emergency department crowding on reassessment of children with critically abnormal vital signs. Acad Emerg Med. 2014; 21(10): 1116–20.
6. Lambe K, Currey J, Considine J. Frequency of vital sign assessment and clinical deterioration in an Australian emergency department. Australas Emerg Nurs J. 2016; 19(4): 217–22.
7. Kagiyama N, Hiki M, Matsue Y, et al. Validation of telemedicine-based self-assessment of vital signs for patients with COVID-19: a pilot study. J Telemed Telecare. 2023; 29(8): 600–6.
8. Glazkova N, Podladchikova T, Gerzer R, et al. Non-invasive wearable ECG-patch system for astronauts and patients on earth. Acta Astronaut. 2020; 166: 613–8.
9. Selvaraju V, Spicher N, Wang J, et al. Continuous monitoring of vital signs using cameras: a systematic review. Sensors. 2022; 22(11): 4097.
10. Di Rienzo M, Vaini E, Lombardi P. Development of a smart garment for the assessment of cardiac mechanical performance and other vital signs during sleep in microgravity. Sens Actuators A Phys. 2018; 274: 19–27.
12. Latten GH, Spek M, Muris JW, et al. Accuracy and interobserver-agreement of respiratory rate measurements by healthcare professionals, and its effect on the outcomes of clinical prediction/diagnostic rules. PLoS One. 2019; 14(10): e0223155.
13. US Food and Drug Administration. “Re: K211926” Accessed 06/19/2024. https://www.accessdata.fda.gov/cdrh_docs/pdf21/K211906.pdf.






Join the Conversation